New C-NACHE research project begins
C-NACHE is excited to announce the start of a new cancer health equity research project within our center titled “Improving Breast and Cervical Cancer Screening for Native American Women with Intellectual and Developmental Disabilities (IDD)” and led by co-principal investigators (PI) Dr. Darold Joseph and Dr. Julie Armin.
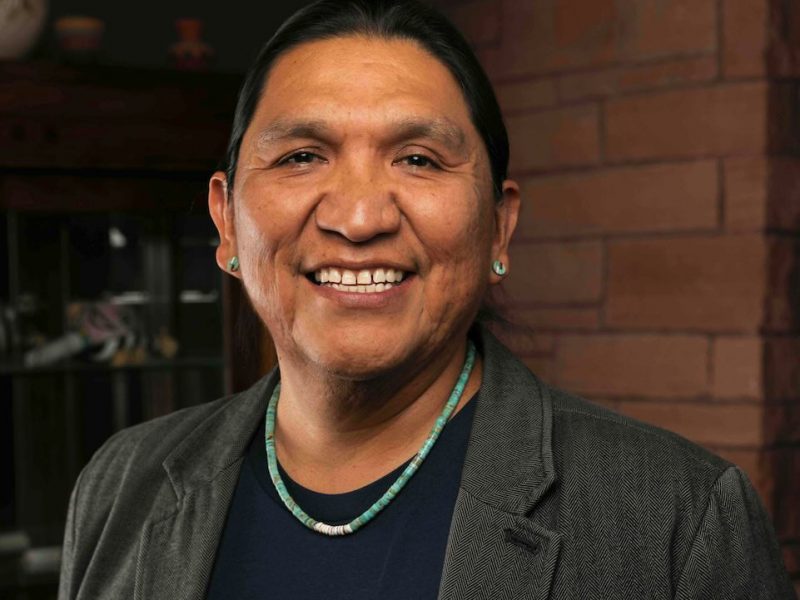
 Dr. Darold Joseph and Dr. Julie Armin with Devine Holmes and Jessica Onsae at the American Indian Disability Summit in April 2024.
Dr. Darold Joseph and Dr. Julie Armin with Devine Holmes and Jessica Onsae at the American Indian Disability Summit in April 2024.
This project aims to address the social determinants of health related to education and social context by enhancing reproductive health knowledge among women with IDD and evaluating how caregiver and institutional settings impact access to cancer screenings. The project will also explore policy and practice factors to improve cancer screening interventions, focusing on testing the effectiveness of the My Health My Choice (MHMC) program for Native American women with IDD and identifying influences on screening uptake using the Consolidated Framework for Implementation Research (CFIR).
Specific aims of the project include:
- Aim 1: Conducting a wait list control trial of MHMC, examining increased cancer screening receipt among Native American women with IDD and their caregivers.
- Aim 2: Explore the dimensions of relationships between caregivers/supporters and women with IDD in preparation for an examination of the relationships’ effects on screening decision-making.
- Aim 3: Identify multi-level factors relevant to the promotion of real-world uptake of the MHMC within disability- and native-serving agencies.
This project aligns with the overall goals of C-NACHE to improve cancer screening rates among Native Americans, while also addressing the needs of a largely underserved cancer health equity group, Native American women with IDD.
To learn more about the amazing cancer researchers behind this impactful project, read the Q&A below.
C-NACHE principal investigators

Q&A section
Question topics: Research Journey, Breakthroughs and Discoveries, Challenges and Solutions, Collaborative Efforts, Advancements in Technology, Community-Centered Research, Education and Awareness, Future Directions, and Personal Reflections.
Q: What inspired you to pursue a career in cancer research?
A: “My inspiration to engage in research stems from growing up in the rural Village of Moenkopi and small town of Tuba City. My lived experiences have led me to understand that Indigenous strengths and assets from a cultural lens are always accessible and available but not often represented in research engaging Indigenous communities. This lens has led me to pursue research that addresses the educational/health inequities and disparities existing in our communities that affect the health and well-being of individuals with and without disabilities. Conducting cancer prevention research with my colleague and Co-PI Dr. Julie Armin, is an example of this with our project titled, “Improving Breast and Cervical Cancer Screening for Native American Women with Intellectual and Developmental Disabilities (NAWwIDD)”, aimed to provide culturally responsive cancer screening education and navigation practices for NAWwIDD to increase breast and cervical cancer screening among this population.” – Dr. Joseph
A: “Before I decided to attend graduate school, I worked for the American Cancer Society as a Media Relations Manager. In that position, I was lucky enough to work with and learn from many of the community-focused staff and volunteers. They educated me about the inequities in cancer care access that exist in the U.S. These insights drove and continue to drive my interest in studying ways to improve communities’ connections to cancer care services.” – Dr. Armin
Q: What has been the most significant breakthrough or discovery in your research and what are the impacts?
A: “Our project is unique in that we have community partnerships with the Hopi Nation Cancer Support Services Program and the Tucson Indian Center who are both geographically unique, being located in both the rural and urban southwest, respectively. Through our partnerships we’ve learned more about the critical necessity of intentionality to adapt procedures and practices that are responsive to the cultural contexts for each community. For example, accessibility to health care services is vastly different considering the availability of options to choose from to receive healthcare. Additionally, the translation of medical terminology in culturally relatable ways using Indigenous language and context is important.” – Dr. Joseph
A: “My most significant discoveries often highlight the importance of everyday activities of professionals caring for patients and of people living with cancer. In one study, I qualitatively documented the “works of illness” performed by uninsured patients with cancer. The works of illness refer to all the work people with a particular health concern perform in the service of their cancer treatment or to maintain their well-being and the well-being of their families and networks. This might not be the kind of work that lands on the cover of Nature, but it can potentially influence health care policies and priorities! In fact, I am currently working with colleagues on a project to build capacity for communities (professionals, institutions, community organizations) to address the needs of uninsured cancer patients.” – Dr. Armin
Q: What are some of the major challenges you face in your research, and how do you overcome them or adapt to them?
A: “The inequities and disparities effecting the rate at which women with intellectual and developmental disabilities complete breast and cervical screening greatly impact the resources available to build health literacy. Even more so when considering the intersects of disability with cultural contexts.” – Dr. Joseph
A: “The most significant challenge I experience is ensuring sustainability for projects, which generally requires ongoing funding. This sustainability is especially important for projects that include and engage communities.” – Dr. Armin
Q: How important is collaboration in cancer research, and who do you work with (e.g., other researchers, institutions)?
A: “The collaborative climate between our research team members has had a tremendous and positive impact on our cancer research project. Our partners include faculty from Northern Arizona University and the University of Arizona who are Julie Armin (UofA), Janet Rothers (UofA), Chris Segrin (UofA) and Darold H. Joseph (NAU).” – Dr. Joseph
A: “Collaboration is key in cancer research, and major funders like the American Cancer Society and the National Institutes of Health realize this, so they prioritize collaboration. I work with researchers that have expertise in areas that are complementary to my own – whether in subject or methods—and I also work with community partners toward cancer health equity. Working with community partners means that their priorities might not be my priority as a researcher, and this generates creative solutions to challenges and research results that are meaningful and useful for communities.” – Dr. Armin
Q: How do you involve community in your research, and why is community involvement important?
A: “Our project continues to focus on utilizing community based participatory and Indigenous research practices. For this reason, we maintain collaborative relationships with the Hopi Cancer Support Services program and the Tucson Indian Center.” – Dr. Joseph
Q: How do you educate others about your research and its implications?
A: “The My Health My Choice (MHMC) project includes the formation of a community advisory board made up of medical and service providers with experience serving Indigenous communities. Through our meetings with the CAB, we provide education and updates about our project. We also maintain the MHMC website at https://www.myhealthmychoice.org to provide education and awareness to the broader community.” – Dr. Joseph
A: “I take the opportunity to share my research with academic audiences as much as possible, but also to share with various types of communities (e.g. communities who are the “subjects” of study, public health communities). For instance, I try to participate on statewide health committees so that I can share my expertise and use my own—or others’—evidence to influence the public conversation. I appreciate the opportunity to share with communities of interest to learn how they understand my research and how they see the research’s usefulness for them.” – Dr. Armin
Q: What excites you most about the future of your cancer research?
A: “I am excited about taking the next steps with the MHMC project to explore the role and impact of caregivers/supporters on cancer screening for Native American women with IDD. In my years of experience serving individuals with disabilities, particularly individuals with IDD, I have observed the role and critical value of having a caregiver/supporter to increase the quality-of-life outcomes for people with IDD. I mainly have made these observations in educational and employment related spaces and am excited to learn more about the ways our project team will learn from caregivers/supporters to address cancer prevention.” – Dr. Joseph
A: “I’m excited by the opportunity to use the evidence we already have about health services delivery to improve cancer care for communities that have been historically marginalized. I see cancer research and social justice as inextricably linked.” – Dr. Armin
Q: Can you share a memorable moment from your research journey that has stayed with you?
A: “I continually am reminded about the value of maintaining an Indigenous Hopi perspective about my relationality to community and the histories, languages, ceremonies, and lands the communities I engage with, are connected to. I say this because it has always sustained a value of responsibility in research and reciprocating to our Indigenous communities. For example, in a project which a report back to an Indigenous community was taking place, to a group of elders, the elders indicated how it was important to have our “own” Indigenous people doing health research because they understand the community. These types of experiences keep me grounded to why I have participated in conducting research.” – Dr. Joseph
A: “On the My Health My Choice project, we use a consent form that includes “teach-back” questions to ensure participant understanding of the study procedures, the risks and benefits, and their responsibilities and rights as a participant. We added these questions as a “best practice” for gaining consent from participants with intellectual and/or developmental disabilities. However, as a team, we decided to use the teach-back questions for all participants, whether or not they identified as having a disability. When using the teach back questions, I found that many people may not understand the basic information of the study. The teach-back questions enable the researcher to return to important parts of the consent and ensure that everyone has a clear understanding of the study. I now want to use them with every study!” – Dr. Armin