Exploring Native American Cervical Cancer Disparities through the Lens of the Vaginal Microbiome
Co-leaders: Melissa Herbst-Kralovetz (UACC); Naomi Lee (NAU); Greg Caporaso (NAU)
Approximately 11,000 new cases of cervical cancer were diagnosed in the U.S. in 2018. While the cervical cancer mortality rate declined, approximately 4,000 women still die from this disease every year. According to Indian Health Service data from 1999-2009, Native American (NA) women had approximately a two-fold higher incidence in cervical cancer and associated mortality rate than white women. White Hispanic and NA women have the highest rates of cervical cancer in Arizona (AZ), with 8.4 cases per 100,000 NA women. While HPV is the known etiologic agent of cervical cancer, few studies were conducted to estimate HPV prevalence within NA communities. Among those studies, it was reported that 22.2% of NA women from the Hopi reservation in northeastern AZ tested positive for HPV infection. The deficiencies of both cervical screening and higher HPV prevalence are likely contributors to cervical cancer disparities among NA women, however other factors include the vaginal microbiome may contribute to persistence and progression of cancer.
Despite differences in cervical cancer rates between racial and ethnic groups, little is known about the patterns of HPV infection, the composition of the vaginal microbiome in NA communities, or how these factors relate to increased cervical cancer risk. In fact, most prior studies do not include NA women, therefore there is a critical unmet need for these women to be included in studies.
To address this need, our collaborative team is dedicated to disseminating information on cancer screening, HPV vaccination, and women’s health to the NA community. We have demonstrated this commitment through a culturally tailored video production with our partners at the Native Americans for Community Action clinic on women’s health that was widely disseminated on social media. Despite the COVID-19 pandemic, we saw an increase in recruitment after the dissemination of the video. We continue to work with the clinic to develop new recruitment strategies for the project along with educational information for healthcare providers. For example, the research team provided culturally informed educational sessions NA-serving healthcare providers on the importance of the vaginal microbiome and cervical cancer. The full project will continue these efforts in collaboration with the NACP Outreach Core. To reach a broader cohort, the full project will expand to the greater metropolitan Phoenix area in partnership with MedStar Health Research Institute (MHRI). Finally, additional education efforts are planned in collaboration with the Education and Outreach Cores, and through Lee and Caporaso’s Chan-Zuckerberg Initiative funded K-12 scientific computing education and outreach program, the Four Corners Science and Computing Club, which is focused on schools primarily serving Native American students in the Four Corners region.
Together, we aim to develop a long-term structure to reduce cervical cancer by assessing the vaginal microbiome and HPV longitudinally across all southwest Native American communities.
AIM 1: Expand and implement our culturally informed vaginal sample self-collection protocol for Native American women.
We have ongoing meetings with the MedStar Health Research Institute (MHRI) team in terms of our current protocol and implementation of the biospecimen collection. Training materials for vaginal sample self-collection will be modified on the basis of in-depth interviews with the MHRI research staff. After training with these materials facilitated by the NACP Outreach Core.
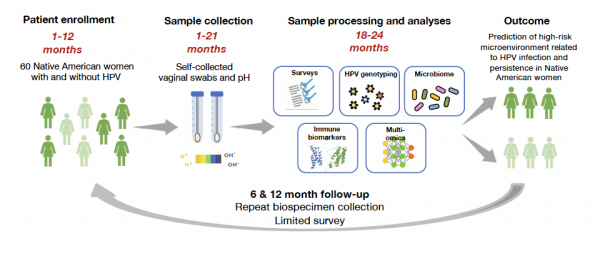
AIM 2: To establish the feasibility of a longitudinal self-collection biospecimen protocol among women with and without HPV.
We will conduct a pilot study with 60 Native women to determine the effectiveness of recruitment/retention strategies and the acceptability of the longitudinal biospecimen protocol. An initial questionnaire will be administered to these participants enabling assessment of associations between the VMB and HPV types with sociodemographic factors, sexual history, knowledge of safe sex practices, and health behaviors. All women will be provided kits to take home during their initial visit. Participants will be instructed to return the kits at 6 and 12 months for a total of 3 longitudinal specimens/participant. A short questionnaire on acceptability, health, and sexual history will be returned to the research team with both at-home kits.
AIM 3: Correlate the vaginal microbiome composition, host immune activity, HPV genomes, and Lactobacillus abundances in Native American women to better understand the relationship between these factors and HPV infection.
Women will be stratified into two groups based on their HPV status (i.e. negative vs. positive for any high-risk HPV genotype). 16S microbiome sequencing-based VMB profiles, vaginal pH, 12 immune mediators (cytokines, chemokines, growth factors and other immune biomarkers), HPV genotype, and Lactobacillus abundance data will be generated from the vaginal swabs collected in Aim 2. Associations between these features and cervical epithelial status—normal or infected with high-risk HPV will be investigated with biostatistics assistance (Dr. Roe) through the NACP Administrative Core.